New Ways To Save Your Brain During Stroke

Find Your Perfect Match
Answer a few questions and we'll provide you with a list of primary care providers that best fit your needs.
If you or a loved one has a stroke, you need immediate medical attention to restore blood flow and oxygen to your brain. The sooner you receive treatment, the less your risk of permanent brain injury, disability, or death.
The good news: The chance you’ll receive timely treatment of stroke is greater today than ever before. New technology and advances in stroke treatment systems make this possible.
Faster Care, No Matter Where You Live
 Technology is opening the way to more immediate stroke treatment, even if you live in a remote area, away from major medical facilities that are staffed by physicians trained in stroke treatment.
Technology is opening the way to more immediate stroke treatment, even if you live in a remote area, away from major medical facilities that are staffed by physicians trained in stroke treatment.
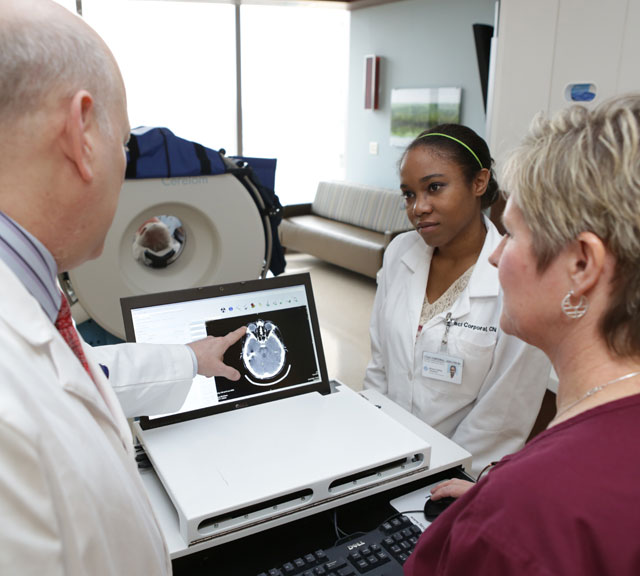
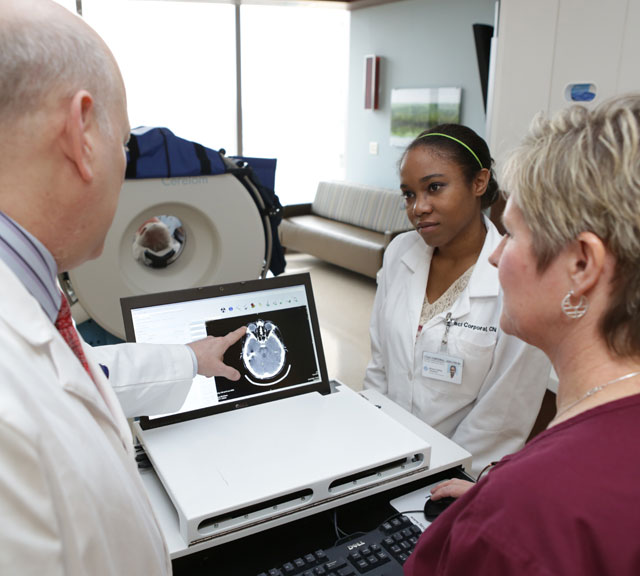
TeleStroke networks, such as Premier Health’s, provide 24/7 access to teams of stroke specialists via the internet. TeleStroke virtually links the specialists with emergency medical personnel as they treat patients in hospitals without stroke-trained physicians.
Using video equipment, an internet connection, and other technology, the off-site specialists can quickly evaluate the patient. And they partner with the emergency medical team to treat the patient to minimize the stroke’s effects.
The National Institutes of Health reports that some studies have found that TeleStroke networks help control medical costs and result in more stroke patients being discharged to home from the hospital.
Bryan Ludwig, MD, explains the benefits of TeleStroke networks. “Treatment of stroke is time-dependent. The faster you do it, the better the outcome for the patient.”
“Treatment of stroke is time-dependent. The faster you do it, the better the outcome for the patient.”
Dr. Ludwig talks about TeleStroke.
Click play to watch the video or read video transcript.
TeleStroke is a newer concept in the stroke community. Something that we offer here at Premier, across all of our hospitals. It allows specialized physicians that are trained in identifying stroke and treating stroke to be at the bedside, in virtual terms, so we can speed up care. Telemedicine allows our trained and board-certified, fellowship trained stroke neurologists to transport themselves, if you will, to any bedside, whether it be in our system or within other hospitals that are now connected with our system for this stroke care. As we alluded to earlier, treatment of stroke is all time dependent. And the faster you do it, the better the outcome for the patient. So it made perfect sense that because there are so few trained neurology specialists out there, it's very difficult to have one of these individuals stationed at every hospital that a patient might arrive with stroke symptoms. So we have instead used technology to bring that physician to the bedside via a computer and allow them to both discuss the care with the patient and the patient's family, to examine the patient with the help of the ER physician and the nursing staff at that local hospital. And then make critical decisions on whether they should get IV therapy for stroke, which is a difficult decision to make often times, for those who don't do it frequently. So the stroke doctor is a very critical piece of that team that allows him to say this is somebody that would benefit or identify someone both that may benefit from further therapy like stent retrieval or endovascular therapy for stroke, and would then send a helicopter to bring that patient to the main hospital which offers those surgical treatments of stroke. Or in a third benefit it would be to identify someone who might be part of a research trial that offers a brand-new therapy that isn't able to be offered without this type of interaction and identification quickly of those who might be qualified for clinical trials.
Check a Hospital’s Stroke Credentials
Many hospitals that provide stroke care meet standards that support better patient outcomes. John Terry, MD, explains the two levels of stroke centers established in hospitals around the U.S.
Dr. Terry talks about advanced primary stroke centers, which are certified by The Joint Commission.
Click play to watch the video or read video transcript.
There is an effort in the United States is to systematize or put together systems of care that address patients with stroke. And currently there are two recognized levels of organization. The first is a primary stroke center. A primary stroke center is a healthcare facility that is focused on the rapid evaluation and treatment of stroke patients with the focus on using the blood clot dissolving drug tPA. So these are hospitals that resources have been applied to create a team of physicians and other healthcare workers who are in place and are ready 24 hours a day, seven days a week to identify patients with stroke. Rapidly evaluate them and provide them with tPA, if that is appropriate in that case. And really the idea is to try to get as many patients with stroke who come in and who are appropriate and get them treatment as possible. In the past it's been estimated that there's been as few as 2% of stroke patients that actually were able to get this treatment and over the years, we've seen in centers that are organized and do a very good job, that number can be increased into the 15 to 20% range.
Dr. Terry talks about comprehensive stroke centers, which are certified by The Joint Commission.
Click play to watch the video or read video transcript.
A comprehensive stroke center is the next level of organization that is recognized. And as you might assume from its name, it not only provides the services that are seen in a primary stroke center, but it adds services into that. For ischemic stroke, which is the type of stroke that occurs when a blood vessel is blocked with a blood clot, a comprehensive stroke center is not only able to give intravenous tPA, the clot busting drug, but it also offers the possibility of a procedure where a catheter is inserted into the main artery in the leg and advanced through the arterial system into the brain arteries where the clot is. And then the clot is retrieved using a number of different devices potentially that we currently have to do that. So comprehensive stroke centers are able to do both of those treatments. In addition, the comprehensive stroke treatment emphasizes treatment of the other type of less common stroke, which is called a hemorrhagic stroke. That occurs with a blood vessel breaks or ruptures and bleeding into the brain occurs. These types of strokes may look very similar but the hemorrhagic strokes have fundamentally different treatments that may include things like surgery, very careful blood pressure control and monitoring and care in the ICU. So these types of strokes are included in the scope of care of a comprehensive stroke center.
Advanced primary stroke centers focus on rapid evaluation and treatment of stroke patients. They use the clot-dissolving medication tissue plasminogen activator (tPA) to treat the most common type of stroke, ischemic, in which clots block blood vessels. Nationwide, only 2 percent of patients appropriate for tPA receive the treatment, Dr. Terry says. But this statistic increases to 15 to 20 percent where primary stroke centers are available, he explains.
Comprehensive stroke centers also administer tPA, but add to their treatment capability a clot-retrieval technique, explained below, and techniques to treat less common hemorrhagic strokes that involve blood vessels that rupture in the brain. These techniques include advanced imaging, surgery, careful blood pressure control, and monitoring, and intensive care in the hospital.
Both advanced primary and comprehensive stroke centers must meet specific standards of care and performance measures focused on improved patient outcomes. This includes maintaining a staff of medical professionals specially trained in stroke care.
Comprehensive stroke centers require additional technology and resources to maintain their certification. This includes demonstrated availability of advanced imaging technology and 24-hour availability of staff trained in vascular neurology, neurosurgery, and endovascular procedures.
Comprehensive stroke centers may be at least partially responsible for improving hemorrhagic stroke survival, according to a recent study published in the Journal of the American Heart Association.
Dr. Ludwig describes aneurysm clipping and coiling, procedures that can prevent aneurysms that cause hemorrhagic strokes.
Click play to watch the video or read video transcript.
Aneurysm treatment is broken into two different methods. One is aneurysmal coiling, which is blocking off a weakened spot, that's what an aneurysm is. Going in, through the arteries and blocking off the aneurysm with these little tiny metal wires called coils. And that's what we say when we mean coiling. That procedure and process has been vetted through very significant literature and research. It has been shown to be very effective in treatment of brain aneurysms. The other method is aneurysmal clipping. And that is a way in which a neurosurgeon would go in and open the skull and then put in a very small metal clip across the neck of the aneurysm, this week spot in the artery. So essentially, closing that sack or that weakened pouch off the artery, closing it with this clip so it can't receive blood supply. So both treatments are effective. One is what we call minimally invasive and one is a little bit more invasive. Coiling is minimally invasive and the clipping is more invasive, in terms of you have to open the skull to repair the aneurysm. Both are shown to be safe and both are highly effective in treatment and hopefully cure of brain aneurysms, and we offer both here at this hospital.
A New Procedure: Endovascular Stroke Rescue
In some cases, stroke patients don’t immediately respond to medication therapy. And some patients, due to certain medical conditions, may not be good candidates for tPA drug therapy. In these instances, a new minimally invasive procedure – endovascular stroke rescue – has become the recognized standard of care, says Dr. Ludwig.
Dr. Ludwig explains endovascular stroke rescue.
Click play to watch the video or read video transcript.
Stroke therapy is broken into medical therapy and what we call endovascular stroke rescue. And endovascular has been shown to be the standard of care for patients who don't necessarily respond to medical therapy for stroke in the very early stages. Or even sometimes those who can't receive that medical therapy for various reasons. Stent retrieval has now been proven to be the main method in which to open arteries using noninvasive or minimally invasive surgical techniques to fight stroke. What that means is that you bring wires and catheters through the patient’s arteries. Moving these wires and catheters into the particular artery inside of the brain that has been blocked by a clot. With those same wires and catheters you slip through the clot itself, because it is fairly soft material even though it's blocking the artery from getting blood to the brain. You can pass through this clot and then you deploy or push out of these little micro catheter stents that are metal mesh tubes that open up in the artery. They not only return blood supply as soon as you're doing that to the brain that needs it so desperately, but at the same time they work themselves into that clot and they grab it if you will, and so that clot retrieval is retrieving that same stent. A lot of people associate stents with cardiac stents where the physician would go in place a stent and leave it in there. In stroke we actually have stents that are designed to remain attached to the wire that we use to deploy or push the stent out of the catheter. We can then pull that stent out through the artery and with it comes the clot. Which allows blood supply to get to the brain and hopefully reverse the stroke.
A doctor threads a catheter through an artery in the groin, up to the blocked artery in the brain. The catheter moves a stent, a wire-caged device, to the blockage. The stent opens, grabs the clot, and the doctor removes the stent with the trapped clot.
This procedure can be done up to 24 hours after stroke symptoms begin.
In 2018, the timeframe for this procedure expanded from six to 24 hours after stroke symptoms begin. Dr. Ludwig discusses the expanded guidelines in this video:
Dr. Ludwig adds that the most recent trial showed that for patients with stroke symptoms starting more than six hours before they arrive at the hospital (but no more than 24 hours from the onset of the stroke) and who qualified for surgical removal of clots, nearly 50 percent were doing well at three months. This was compared to similar patients who didn't receive the surgery, where only 13 percent of patients were doing well three months after their stroke. And timely treatment is more likely now due to stroke care innovations such as TeleStroke and advanced and comprehensive stroke care centers.
Find Your Perfect Match
Answer a few questions and we'll provide you with a list of primary care providers that best fit your needs.
Source: American Stroke Association; Bryan Ludwig, MD, Premier Health Clinical Neuroscience Institute; John Terry, MD, Premier Health Clinical Neuroscience Institute

 Technology is opening the way to more immediate stroke treatment, even if you live in a remote area, away from major medical facilities that are staffed by physicians trained in stroke treatment.
Technology is opening the way to more immediate stroke treatment, even if you live in a remote area, away from major medical facilities that are staffed by physicians trained in stroke treatment.










