Surviving the Sepsis-3 Conundrum
 By Andrew Maigur, MD, system director, Physician Advisor Program
By Andrew Maigur, MD, system director, Physician Advisor Program
Disclaimer: “The accurate diagnosis of Sepsis is not for Diagnosis Related Group (DRG) assignment, increased reimbursement, or improved quality metrics. The prompt diagnosis and treatment of Sepsis is first to improve medical care and outcomes of patients.”
Before we jump into the Sepsis-3 definition, let’s start with what we know so far about Sepsis: the all-too-familiar Sepsis 1 and 2 definitions and systemic inflammatory response syndrome (SIRS) criteria (SIRS plus source of infection equals Sepsis; and Sepsis plus acute organ dysfunction equals severe Sepsis). As of today, the Centers for Medicare and Medicaid Services (CMS) continues to follow the antiquated Sepsis 1 definition for the Sepsis core measure bundle. What resulted was a misinterpretation; what was meant to be a screening tool for SIRS became a diagnostic criterion. Clinicians and Clinical Documentation Improvement (CDI) specialists forgot that Sepsis mandates that the patient is sick with a capital “S.”
Sepsis-3 defines Sepsis as a life-threatening organ dysfunction caused by a dysregulated host response to infection. In other words, sicker than the average patient with the localized infection. Integral to this definition of Sepsis is acute sepsis-related organ dysfunction.
Enter the Third International Definition for Sepsis and Septic Shock in February 2016. It was only in 2017 that the Surviving Sepsis Campaign (SSC) adopted the definition of Sepsis-3 and effectively removed all references to SIRS from their literature. Needless to say, the Sepsis-3 definition has been wrapped in controversy with a lot of debate and has ultimately been endorsed by the Centers for Disease Control and Prevention (CDC), American College of Emergency Physicians, and the Society of Critical Care Medicine (SCCM).
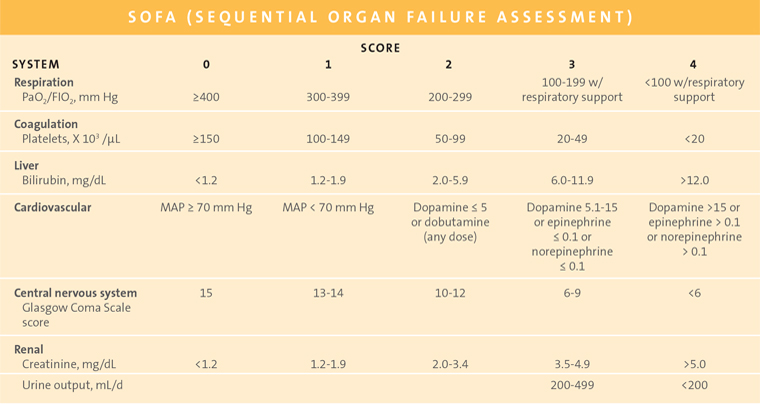
What about Sequential Organ Failure Assessment (SOFA)? SOFA and qSOFA are tools designed to prognosticate mortality in the ICU patient, but they are not intended to be the definitive clinical criteria for diagnosis.
A few comments on the SOFA score; the bar is pretty low for a positive SOFA score greater than 2. The score is based on a change from baseline (acute sepsis-related organ dysfunction). The presumption is that the score is 0 if there is no previously known organ dysfunction. If the patient has organ dysfunction at baseline, the score is determined by the change in strata. There are organ dysfunctions that are not found in SOFA but could be supportive of sepsis. These include (acute sepsis-related) ileus; Type 2 myocardial infarction (MI); critical illness neuropathy or myopathy; toxic epidermal necrolysis (from infection, not from medication); and liver dysfunction such as transaminitis (without hyperbilirubinemia).
Quick SOFA (qSOFA) was meant to be an easily-obtained-at-the-bedside surrogate for the SOFA score, which requires blood work results. The criteria are:
- Respiratory rate ≥ 22/minute (so nurses who guestimate 18 or 20 won’t trigger qSOFA)
- Altered mentation (think ENCEPHALOPATHY!)
- Systolic blood pressure ≤ 100 mm Hg
There are six things that the provider should consider regarding a sepsis diagnosis:
- Is there a presumed or confirmed infection? Is it documented in a codable format?
- Is the patient sicker than the average patient with the localized infection?
- Is there organ dysfunction due to the sepsis?
- Linkage must be to sepsis and not to the alternate diagnosis, e.g., “AKI due to dehydration.”
- The SOFA score can be supportive if ≥ 2. If not, the provider should acknowledge and document thought process.
- Can the coder pick up the code for “severe sepsis”?
- All sepsis is the condition formerly known as Severe Sepsis.
- The combination of “sepsis” and acute sepsis-related organ dysfunction is adequate support for Severe Sepsis.
- Are the core measures being attended to?
- Core measure bundle should be performed on all patients with “sepsis” (formerly known as Severe Sepsis).
- SIRS can prompt you to consider Sepsis and assess for organ dysfunction but is not singular grounds for making the diagnosis.
What are some of the tools for your tool belt to assist in documenting Sepsis accurately in the medical record?
- The Sepsis dot phrase – .Sepsis3 – created by EPIC programmers makes documenting easy with drop down menus. Example: Sepsis due to [infection] with acute sepsis-related organ dysfunction as evidenced by [specify organ dysfunctions].
- A SOFA score calculator is currently being built into the Scoring tools in EPIC.
- Make sure the diagnosis carries through the record from the time of diagnosis to the discharge summary with consistent documentation by all providers.
- Use uncertain diagnosis (possible sepsis) – It’s better to entertain early and make an uncertain diagnosis and rule out, than to miss the diagnosis.
- The patient either has Sepsis (life-threatening organ dysfunction caused by dysregulated host response to infection) or they do not; there is no code for “early,” “impending,” or “aborted” sepsis.
- Avoid “multiple system organ failure.” That can’t be coded. List the organ dysfunctions.
- Avoid sepsis-adjacent phrases like “urosepsis,” “early sepsis-like pattern,” meets “sepsis criteria,” and “sepsis syndrome.”
- Providers should tell the story longitudinally and avoid contradictory, conflicting, or flip-flopping documentation.
In today’s payer denial environment, Sepsis is nationally a diagnosis most prone to audits and denials. Payers can deny a diagnosis up to five years after discharge, which leads to a DRG downgrade and reimbursement recoupment from hospitals. So far, UnitedHealthcare is the only payer that has officially announced they have adopted the Sepsis-3 definition. Most other payers are citing Sepsis-3 definition criteria in their denial letters, hence the importance of defensive documentation in the medical record.
Providers, without a doubt you take excellent care of patients, but you need to document well to get credit for having done so. You want the patient to look as sick and complex in the medical record as they appear in real life. Happy Documentation!!
References:
Singer M, Deutschman CS, et.al., The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3), JAMA, 2016;315(8):801-810. https://jamanetwork.com/journals/jama/fullarticle/2492881
Surviving Sepsis Campaign, website: http://www.survivingsepsis.org/Pages/default.aspx
Remer EE, Payers and Clinicians Should use Clinically Accepted Criteria When Diagnosing Sepsis, January 29, 2019 https://www.icd10monitor.com/payers-and-clinicians-should-use-clinically-accepted-criteria-when-diagnosing-sepsis
Remer EE, Warning: All Sepsis is Severe Sepsis, icd10monitor.com, September 12, 2017 https://www.icd10monitor.com/warning-all-sepsis-is-severe-sepsis
American College of Physician Advisors, CDI Subcommittee, Sepsis Information for Physician Advisors.
Back to the September 2019 issue of Premier Pulse

