Understanding Vizient’s Risk Adjusted Index
 By Andrew B. Maigur, MD, system director, Premier Physician Advisor Program
By Andrew B. Maigur, MD, system director, Premier Physician Advisor Program
Do the data collected by health care systems truly represent the patient I am caring for? They can, and physician documentation is critical to truly capture all major comorbidities, which then translates into coded data and affects your quality metrics, giving you credit for the high-quality care provided at the bedside. While reimbursement matters, accurate, compliant, and complete documentation opens the door for the patient to receive all the care needed for each episode.
Centers for Medicare and Medicaid Services (CMS) moved away from volume-based care to value-based care and created the hospital value-based purchasing program (HVBPP). CMS currently defines value-based care as paying for health care services in a manner that links performance to cost, quality, and the patient's experience of care. The HVBPP consists of 30-day risk-adjusted mortality measures and health care associated infections. The program is funded by reducing participating hospitals’ base operating Medicare Severity Diagnosis Related Group (MS-DRG) payments by 2% based on performance as compared to other providers. Essentially the hospital’s downside risk is up to a 2% penalty, while the upside gain can be a 2% bonus which can translate into millions of dollars of reimbursement.
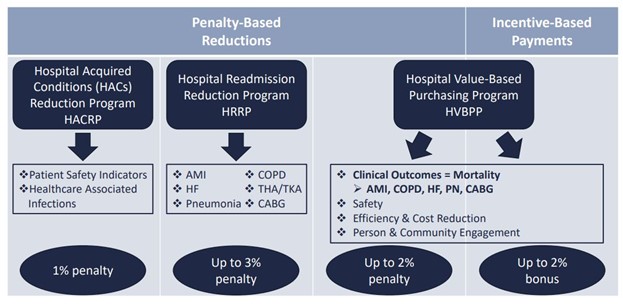
Fig 1: CMS Quality & Value Based Programs
Vizient, a national organization, provides participating health systems with detailed quality data benchmarked to comparable size and acuity health systems. Vizient's quality metrics align with and affect the CMS Star Quality measures, including HVBPP and many others. Vizient's clinical database provides three important metrics: Length of Stay (LOS) index, Mortality index, and Cost index. Each index is primarily a ratio of observed-over-expected values for a particular patient population. The observed (or numerator) is determined by care quality and patient characteristics, and the expected (or denominator) is primarily determined by documentation based on the patient's diagnosed conditions. An index of < 1 represents an excellent quality outcome with the expected exceeding the observed and an index of ≥ 1 where the observed exceeds the expected may indicate an opportunity for quality improvement or a need for improved documentation. Their risk adjustment methodology identifies certain variables that carry a higher weight, which translates into a sicker patient, utilizing increased resources (LOS, cost), and an elevated risk of poor outcomes (mortality). The concept of “denominator management” represents capturing multiple accurate risk variables, which in turn increases the expected value – hence driving the index lower, i.e., less than 1. Dementia and CHF are the only risk variables that are not required to be Present on Admission (POA).

Fig 2: Examples of high weighted risk variables.
As an example, the malnutrition risk variable includes a family of International Classification of Diseases (ICD-10) diagnosis codes for mild/moderate or severe protein calorie malnutrition, adult failure to thrive, cachexia, and obesity. This risk variable carries a high weight impacting Mortality, LOS, and cost index by increasing the "expected/denominator" value. For a specific diagnosis to be accounted for in the risk adjustment methodology, the present on admission status of that diagnosis is crucial. For the above-stated diagnoses, if they are documented as present on admission (POA = Yes) or clinically unable to determine POA status, the diagnosis will qualify as a risk variable. Therefore, it is crucial to accurately capture all risk variables within 24 hours of an inpatient admission.
Vizient has identified opportunities for Premier Health with increased capture of the following top five risk variables:
- Malnutrition
- Fluid and electrolyte disorders
- Blood loss/nutritional/anemia of chronic disease
- Coagulation defect
- Metastatic cancer
Denominator management includes both prospective and retrospective interventions. Prospective interventions are focused on education to provider groups to increase the capture of high weighted risk variables across all inpatient admissions at our facilities. Retrospective interventions focus on retrospective chart reviews identifying missed risk variable capture opportunities that lead to quality/clinical documentation/coding/Physician Advisor queries to the providers for clarification.
At Premier Health, our Quality/CDI/Coding and Physician Advisor Teams are working on retrospective interventions focused on Mortality reviews. We have started prospective education with the hospitalist and pulmonary critical care groups.
Please feel free to reach out directly to me for additional information at abmaigur@premierhealth.com.
References:
CMS Value Base Care hrsa.gov
Back to the March 2023 issue of Premier Pulse

