Polyps: Colorectal Cancer’s Early Warning System
Find Your Perfect Match
Answer a few questions and we'll provide you with a list of primary care providers that best fit your needs.
What’s a polyp? What’s it doing in your colon? And why should you have it removed? You’ve probably heard about polyps. You may know someone who has had one (or more!) But you’ll want to know more to protect yourself from a risk of developing colorectal cancer.
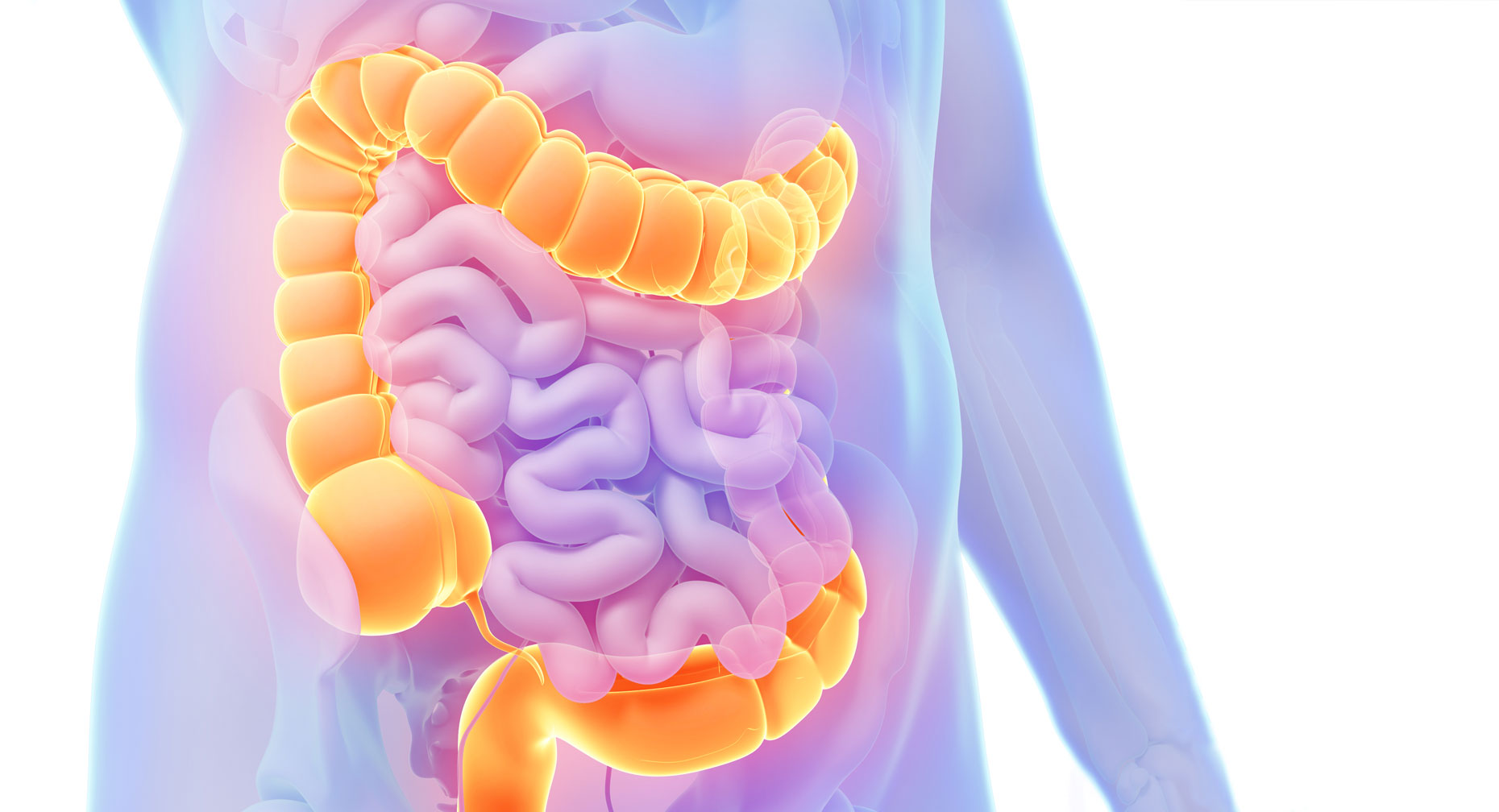
A polyp is a fleshy clump of tissue that can develop on the smooth, inner lining of your colon or rectum. In some cases, the tissue appears flat. Polyps rarely occur in young people, but the average 60-year old with no particular risk factors for polyps has a 25 percent chance of having one or more polyps.
In addition to age, the biggest risk factor for developing polyps is a family or personal history of polyps. Some experts also think that a high-fat, low-fiber diet contributes to their formation.
Most polyps are completely harmless, but they require careful attention because some may develop into colorectal cancer.
Know Your Polyps
There are two main types of polyps:
Hyperplastic — This tissue growth is completely harmless; it does not lead to cancer.
Adenoma — Polyps made of adenoma cells are thought to be the source of nearly all colorectal cancers. Although many of these polyps are totally benign, some carry the risk of becoming cancerous. The longer they are in your colon and the larger they grow, the more likely they are to become cancer.
In addition, there’s a precancerous condition called dysplasia. This means abnormal cells are growing in the lining of the colon or rectum or inside a polyp.
Finding and Removing Polyps
Sometimes, a large polyp will cause bleeding when you have a bowel movement. In most cases, however, you won’t have any symptoms to signal that you have polyps.
The most effective way to find them is through a colonoscopy screening. In this test, a gastroenterologist uses a lighted scope to examine the inner lining of your rectum and colon. Other screening methods that may indicate polyps include testing a stool sample for traces of blood, looking at the lower third of the colon through a sigmoidoscope, taking X-ray pictures using a barium enema dye or using a CT colonography (a virtual colonoscopy) that takes pictures of the inside of the colon without actually inserting a scope into the colon.
Because polyps usually develop during middle age, the American Cancer Society recommends you have your first colonoscopy screening at age 45. Some organizations recommend them at age 45. But if you have inflammatory bowel disease, such as Crohn’s or ulcerative colitis, your doctor may recommend you get a colonoscopy sooner, explains Matthew P. Doepker, MD, with Premier Surgical Oncology. “These diseases increase your risk of developing colorectal cancer. Diverticulitis, on the other hand, doesn’t increase your risk.”
Since your doctor can’t tell a harmless hyperplastic polyp from an adenomatous polyp just by looking at it, the safest course is for your doctor to remove all polyps with small cutting instruments during a colonoscopy. The lining of the colon doesn’t have sensitive nerve endings, so there is no pain or discomfort.
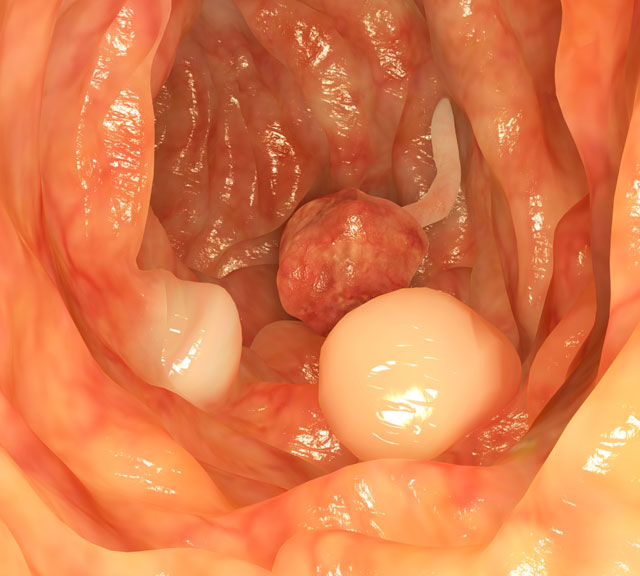
A lab will test any tissue your doctor removes to confirm whether the polyp is noncancerous or if cancer or precancerous tissue is present.
Reducing Colorectal Cancer Risk
Once you have had polyps removed, doctors generally recommend that you have a colonoscopy within three to five years to check for additional polyp growth. If the polyps were flat against the colorectal lining, your doctor may recommend a colonoscopy sooner to ensure that all polyps were detected and removed.
You won’t have any symptoms to signal that you have polyps.
It’s important to find polyps because of the chance that they may transform into colorectal cancer and invade deeper layers of the colon or rectum. Early removal of polyps reduces the risk of cancer growing and spreading to lymph nodes or nearby organs, such as the liver.
“If polyps are found during one of your early colonoscopy screenings, you can expect that polyps may be found at subsequent screenings,” says Dr. Doepker. “This is partly due to your diet, but also to genetics.” He recommends a healthy diet that includes plenty of fiber. And if your family has a history of colorectal cancer, be sure to let your doctor know.
As with many cancers, the earlier you treat colorectal cancer, the more effectively it can be contained and cured.
Find Your Perfect Match
Answer a few questions and we'll provide you with a list of primary care providers that best fit your needs.
Source: American Cancer Society; American Society for Gastrointestinal Endoscopy; Matthew P. Doepker, MD, Premier Surgical Oncology





